E/M codes may report evaluation and management services either alone (pharmacological/ medical management and no other service reported that day) or with the addition of psychotherapy. Psychotherapy is reported as an “add-on” code to the primary procedure, the E/M service. This change effectively reverses “psychotherapy with or without E/M” to “E/M with or without psychotherapy.” The parameters of psychotherapy, such as time, presence of interactive complexity, and site of service, are discussed below. For additional information, go to the AACAP website. For 2021, E/M code selection has been revised. Codes are selected on the basis of time or medical decision-making, and documentation requirements have been streamlined to capture the criteria used for code selection. Additional webinars discussing these revisions, along with clinical vignettes and Summary Guides are also available at the link above.
What is a “new” patient?
Using new patient E/M codes (99202 to 99205) is more restrictive than using psychiatric diagnostic evaluation codes (90791, 90792; described in the following section.).New patients must not have received any professional services in the past three years by the physician OR another physician in the same group practice of the exact same specialty and sub-specialty. Advanced practice nurses, physician assistants and covering professionals working with physicians are considered as working in the exact same specialty and exact same sub specialties as the physician.
Determining Evaluation and Management (E/M) by Time (Outpatient)
Time can be used to select the level of E/M services. Time is calculated based on all services rendered during the 24-hour day of service. This includes face-to-face services and non-face-to face services. Non face-to-face services include charting, telephone contact with others involved in the patient’s care, verbal orders, review of records and labs, insurance authorizations, etc. (See chart below for time units). Documentation should include the topics discussed to support the amount of time for the code selected.
Documenting Time in your encounter note
Documenting time spent in a medical note is crucial for ensuring accurate record-keeping and billing. Here are key steps to consider:
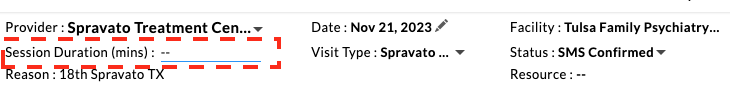
- Specify the Total Time: Clearly state the total amount of time spent with the patient. This includes face-to-face time for outpatient visits and unit/floor time for inpatients. – In Charm, you can also make use of the session duration field at the top of your note by entering total mins.
- Break Down the Time: If applicable, break down the time into different components, such as time spent reviewing tests, discussing treatment options, or coordinating care.
- Describe the Nature of the Time Spent: Detail the nature of the work done during this time. For instance, counseling or coordination of care, explaining test results, or discussing treatment options.
- Use Standard Time Units: Record the time in standard units (minutes or hours). Avoid vague terms like “a short time” or “an extended period.”
- Link Time to Specific Activities: Connect the time spent to specific activities or discussions. This makes it clear that the time was necessary and directly related to patient care.
- Include Start and End Times: For more detailed documentation, include the start and end times of the session. This is particularly important for procedures or longer consultations.
- Document Time Spent Outside of the Encounter: If you spend significant time outside of the direct patient encounter (like reviewing records or coordinating care), document this separately, specifying what was done.
- Be Consistent with Billing Codes: Ensure that the time documented aligns with the billing codes used. Different codes have different time requirements.
- Maintain Privacy and Confidentiality: While documenting time, be mindful of patient privacy and confidentiality. Avoid including unnecessary personal details.
- Review and Update Regularly: Regularly review your documentation practices and update them as needed to stay in line with current guidelines and regulations.
Remember, accurate time documentation not only supports billing and compliance but also enhances the quality of patient care by providing a clear picture of the care process.
Prolonged Service With or Without Direct Patient Contact on the Date of an Office or Other Outpatient Service (99417 & G2212)
99417 is used to report prolonged total time provided by the physician or other qualified health care professional on the date of office or other outpatient services (i.e., 99205, 99215) when that code has been selected on the basis of time. To report a unit of 99417, 15 minutes of additional time must have been attained based on the minimum time required to report the highest-level service.
Please note that Medicare is currently not recognizing this code. Individual payers may differ in their reimbursement policies. For examples of coding with 99417, please see AACAP’s Summary Guides, here.
Two new prolonged service codes were created for use when outpatient E/M services exceed each 15 minutes beyond the highest level E/M code (99205, 99215). One is for use with Medicare patients (G2212) and the other is a CPT code (99417). Check with your non-Medicare payers to determine which to use and check the specific requires for use which vary between the two codes.
Prolonged Service Without Direct Patient Contact (99358, 99359)
Codes 99358 and 99359 describe prolonged, non–face-to-face time personally spent by the physician or other qualified health care professional before or after a related E/M encounter, beyond the usual work inherent in the E/M service.
While these codes remain valid in CPT, they have not demonstrated reliable reimbursement across most commercial payers and are not payable under Medicare FFS. As a result, they should be viewed as descriptive codes rather than dependable revenue drivers.
Some necessary psychiatric work, particularly coordination, record review, and complex clinical synthesis, is not reliably reimbursed under current fee-for-service structures.
We will bill cleanly, defensibly, and realistically, using the tools that actually pay, while acknowledging the limits of the system.
E/M Time-Based Coding Quick Reference (2024)
New Patients (99202–99205)
| Code | Level | Minimum Time | MDM | When to Add Prolonged Services |
|---|---|---|---|---|
| 99202 | 2 | ≥15 min | Straightforward | Not applicable |
| 99203 | 3 | ≥30 min | Low | Not applicable |
| 99204 | 4 | ≥45 min | Moderate | Not applicable |
| 99205 | 5 | ≥60 min | High | If ≥75 min, add 99417 (commercial) or G2212 (Medicare) for each additional 15 min |
Established Patients (99212–99215)
| Code | Level | Minimum Time | MDM | When to Add Prolonged Services |
|---|---|---|---|---|
| 99212 | 2 | ≥10 min | Straightforward | Not applicable |
| 99213 | 3 | ≥20 min | Low | Not applicable |
| 99214 | 4 | ≥30 min | Moderate | Not applicable |
| 99215 | 5 | ≥40 min | High | If ≥55 min, add 99417 (commercial) or G2212 (Medicare) for each additional 15 min |
Key Notes
-
Time includes all provider work on the day of the encounter (face-to-face + non-face-to-face tasks: review, documentation, coordination of care, Rx management, etc.).
-
Exact minutes must be documented in the note (e.g., “Total time 68 minutes: 55 face-to-face, 13 chart review and documentation”).
-
Prolonged services require explicit documentation of the extra time and what was done.
-
Payer differences: Commercial payers usually want 99417; Medicare wants G2212.
Determining Evaluation and Management Levels by Medical Decision Making
Complexity of medical decision making determines the code. The extent of the history and exam are done based on medical necessity and what is appropriate for that visit. Medical decision making is determined by the number of diagnoses that are addressed during the visit, the amount of new data that is reviewed at the visit and the amount of risk involved in the treatment or failure to treat the condition. Treatment decisions included any prescriptions given, and diagnostic studies ordered and any referrals to other health care providers for additional services. Documentation should include the medical thinking and rationale for code selection. Please see AACAP’s tips and principles here.
Psychiatric Diagnostic Evaluation
90791 – Psychiatric Diagnostic Evaluation without medical services
The evaluation may include communicating with family or other sources, as well as reviewing and ordering non-medical diagnostic studies.
90792 – Psychiatric Diagnostic Evaluation with medical services
As above (90791), the evaluation may include communicating with family or other sources, as well as reviewing and ordering diagnostic studies. It must include medical services. “Medical services” refers to “medical thinking” as well as medical activities (e.g., physical examination, prescription of medication, and review and ordering of medical diagnostic tests). Medical thinking must be documented (e.g., consideration of a differential diagnosis, medication change, change in dose of medication, drug-drug interactions). Use of these codes has not changed for 2021.
For both 90791 and 90792:
- In certain circumstances one or more other informants (family members, guardians, or significant others) may be seen in lieu of the patient.
- Both codes may be reported more than once for the patient when separate diagnostic evaluations are conducted with the patient and other informants on different days.
- Use the same codes, for later reassessment, as indicated.
- Do not report on the same day as psychotherapy or an E/M service.
- If present, the interactive complexity component of the diagnostic evaluation is captured by reporting the interactive complexity add-on code 90785 in conjunction with 90791 or 90792.
Do not report with 90839, 90840, 0364T, 0365T, 0366T, 0367T, 0373T, 0374T
Do not report with 99201, 99337, 99341-99350, 99366-99368, 99401-99444, 0368T, 0369T, 370T, 0371T
